More than 10 percent of young and healthy people who develop severe COVID-19 have misguided antibodies that attack not the virus, but the immune system itself, new research shows. Another 3.5 percent, at least, carry a specific kind of genetic mutation. In both groups, the upshot is basically the same: the patients lack type I interferon, a set of 17 proteins crucial for protecting cells and the body from viruses. The findings, appearing in two papers in the current issue of the journal Science, are the first results being published out of the COVID Human Genetic Effort, an ongoing international project involving more than 50 sequencing hubs and hundreds of hospitals around the world. Prof. Tayfun Özçelik, dean of the Faculty of Science at Bilkent University, is a member of the project’s steering committee.
The findings, appearing in two papers in the current issue of the journal Science, are the first results being published out of the COVID Human Genetic Effort, an ongoing international project involving more than 50 sequencing hubs and hundreds of hospitals around the world. Prof. Tayfun Özçelik, dean of the Faculty of Science at Bilkent University, is a member of the project’s steering committee.
“A clear understanding of life-threatening COVID-19 is emerging now. Disruption of type I interferon is central to the process,” says Prof. Özçelik. “Understanding this opens up treatment strategies that rely on interferon.”
The effort is being co-led by Jean-Laurent Casanova at The Rockefeller University in New York City and Helen Su at the US National Institute of Allergy and Infectious Diseases. The participants in the recently published studies included members of various nationalities from Asia, Europe, Latin America and the Middle East.
The way SARS-CoV-2 affects people differently has been puzzling. The virus can cause a symptom-free infection and go away quietly, or it can kill in a few days. Research over the past two decades has shown that unusual susceptibility to certain infectious diseases can be traced to single-gene mutations that affect an individual’s immune response.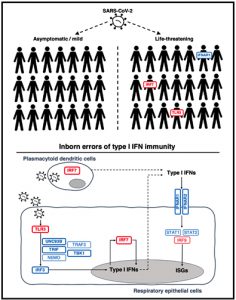 Since February, a team of collaborators has been enrolling thousands of COVID-19 patients to find out whether something in their genetic make-up drives the disparate clinical outcomes the disease produces. The findings that resulted from their investigations help explain why some people develop a disease much more severe than others in their age group—including, for example, individuals who required admission to the ICU despite being in their 20s and free of underlying conditions. They may also provide the first molecular explanation for why more men than women die from the disease.
Since February, a team of collaborators has been enrolling thousands of COVID-19 patients to find out whether something in their genetic make-up drives the disparate clinical outcomes the disease produces. The findings that resulted from their investigations help explain why some people develop a disease much more severe than others in their age group—including, for example, individuals who required admission to the ICU despite being in their 20s and free of underlying conditions. They may also provide the first molecular explanation for why more men than women die from the disease.
Significantly, the findings point to certain medical interventions to consider for further investigation. For example, there are already two types of interferons available as drugs and approved for use to treat certain conditions such as chronic viral hepatitis.
The team continues to look for genetic variations that may affect other types of interferons or additional aspects of the immune response in COVID-19 outliers.
